
Recovering from a critical illness or injury takes time. We can help.
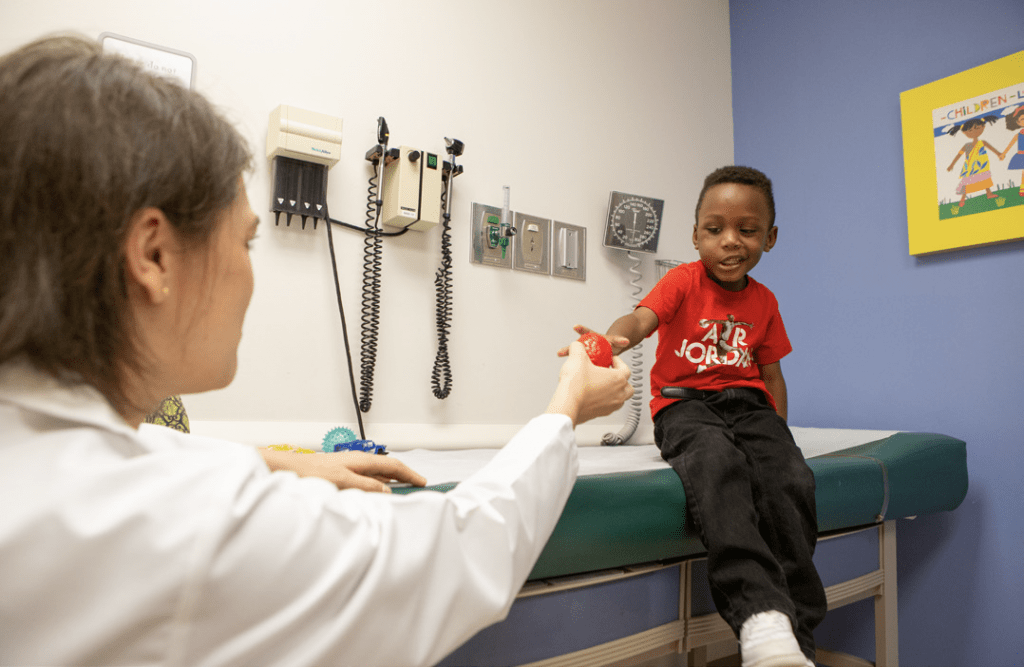
The Neurocritical Care Follow-up Program (NCFP) at St. Louis Children’s Hospital is designed to support your child and family as you transition from the pediatric intensive care unit (PICU) to home.
A serious illness and stay in the PICU can put your child at risk for physical, mental, educational and emotional issues that may slow their recovery. We seek to identify small concerns before they become big ones, so you can connect with resources quickly after discharge.
We work to help your child and family get back to school, work and a regular routine as soon as possible.
Who’s on the team?
We are a team of specialists in neurology, neuropsychology, nursing, social work, education and child development that understand recovery from a serious illness takes time and impacts the entire family.
Families are a central part of our team. We will listen to you, advocate for you, and coordinate closely with your child’s primary care and behavioral health providers, teachers, specialists and community care providers.
How will the NCFP help my child?
After a stay in the PICU, you and your child may face challenges and uncertainties. The NCFP will help you and your child manage:
- Physical and Developmental Changes
- Sleep Concerns
- Attention and Behavioral Changes
- Depression, Anxiety and other Mood Changes
- School and Community Transitions
Who can be part of the Neurocritical Care Follow-up Program?
Children with specific medical conditions or injuries who have stayed in the PICU may be eligible for this program. Conditions include:
- Acute Stroke
- Brain Tumor
- Cardiac Arrest
- Critical illness requiring prolonged sedation
- ECMO Survivorship
- Meningitis/Meningoencephalitis
- Refractory Status Epilepticus
- Traumatic Brain Injury (TBI)

Will my child still have a neurologist and other medical specialties?
Yes! Your primary care provider and specialists will continue to provide ongoing care as needed and be your main contact for clinical care concerns. The NCFP serves as bridge to specialty follow-up and provides additional screening, evaluation, treatment and resources to help your child have the best possible recovery.
When do I get connected with NCFP?
Our special care team starts caring for your child and family while he or she is still in intensive care. We continue to check in with you throughout your child’s hospital stay and after your transition home. Your child’s first appointment with the NCFP will be scheduled for one month after discharge from the hospital.
Questions?
Contact the NCFP team at 314-504-5572 Learn more at StLouisChildrens.org/ncfp
View this information as a PDF (PDF)

Education Liaison Service
Children may have a difficult time returning to school or may experience a decline in school work performance following hospitalization for a serious illness or injury. As part of our mission to provide ongoing support, the Neurocritical Care Follow-up Program (NCFP) has a free educational liaison who will work with you and your child’s school to help make the transition from hospitalization to school as smooth as possible.
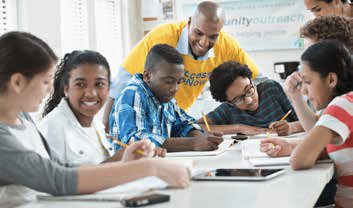
Bringing parents and schools together
The liaison serves as a bridge between you, the hospital and your school to help navigate the transition back to school. We help obtain appropriate educational support and resources for your child. The liaison will work with you and the NCFP team to determine what services your child may need in order to successfully return to school and can assist in ensuring that your child receives those services. Whatever your child’s needs are, the NCFP team is committed to providing the necessary services to help your child succeed.
Parents often wonder:
- How will the school accommodate my child’s needs?
- Do they understand my child’s diagnosis and needs?
Schools have questions, too:
- What kind of accommodations does the child need?
- What activities may the child participate in?
- Are there health needs that should be monitored throughout the day?
- What additional supports and services are needed to best serve this child?
The school liaison helps facilitate communication between parents, the medical team, teachers and school administrators; and together, they advocate for the unique needs of your child.
How does the education liaison help?
Our education liaison:
- Consults with the patient and family about achieving educational and personal goals.
- Communicates with school administrators and teachers about the student’s medical, behavioral, and educational needs.
- Educates school faculty members and staff about the implications of neurocognitive injury.
- Provides information about educational rights and services available through the school system.
- Advocates for accommodations provided through the school district.
- Attends IEP and 504 Plan meetings to support the child’s needs.

For more information or to schedule a meeting
Please contact: Vicki Baker, LPC, Education Liaison, at 314-273-3053 or vbaker@wustl.edu.